The main causes of brain injury include:
Trauma: Head trauma or violent injury can lead to primary or secondary brain damage.
Infections: Brain infections or systemic diseases that spread to the brain can result in impaired brain cell function and brain injury.
Toxicity:Poisoning can cause functional impairments or even cell death in brain cells, leading to brain injury.
Tumors:Tumors in the head or tumors from other parts of the body that metastasize to the brain can lead to brain injury due to the proliferation of malignant tumor cells.
Medications:Some medications can pass through the blood-brain barrier and affect brain cells, causing brain injury.
Hypoxia: Events like drowning, strangulation, or suffocation can cause brain cell hypoxia, resulting in brain injury.
Regarding the effects of hyperbaric oxygen therapy (HBOT) on patients with traumatic brain injury:
Increased Oxygenation: HBOT increases oxygen partial pressure in brain tissues and arteries, thereby raising the overall blood oxygen levels. This helps improve oxygen supply to brain tissues, addressing oxygen deficiency caused by brain injury.
Promotion of Fibroblast Growth and Collagen Formation: HBOT stimulates the growth, division, and formation of collagen fibers, which can promote the reestablishment of collateral circulation. This is beneficial for the recovery of nerve cell function.
Vasoconstriction:HBOT has a vasoconstrictive effect, reducing edema and fluid buildup. This enhances the effective diffusion distance for oxygen, ensuring that even tissues farther from capillaries receive sufficient oxygen. It can also help control brain edema.
Activation of Reticular Activating System:HBOT can activate the brainstem's reticular activating system, enhancing neural activity. This is advantageous for patients with severe traumatic brain injury in regaining consciousness.
Promotion of Neurological Recovery:HBOT may aid in the recovery of neurological functions, reducing long-term neurological deficits or disabilities. It can facilitate the recovery of functions such as speech, memory, and comprehension after traumatic brain injury.
In summary, hyperbaric oxygen therapy is believed to be beneficial for patients with brain injuries by increasing oxygen delivery, promoting cell repair and regeneration, reducing edema, and potentially enhancing neurological recovery. However, the effectiveness of HBOT can vary based on the type and severity of the brain injury and individual patient factors. Decisions regarding the use of HBOT should be made in consultation with healthcare professionals as part of a comprehensive treatment plan.
The inducing factors for brain injury include:
Stroke:Sudden rupture of blood vessels in the brain or blockage of blood flow to the brain can lead to brain hemorrhage or ischemia (lack of blood supply), resulting in oxygen deficiency in brain tissues and extensive brain cell death, causing brain injury.
Heart Disease: Conditions like heart failure and cardiac arrest can lead to insufficient blood supply to the brain, causing oxygen deficiency. Prolonged oxygen deficiency can result in ischemic brain injury.
Neurological Disorders:Neurological diseases can affect the surrounding brain cells and trigger brain injury.
As for why hyperbaric oxygen therapy (HBOT) is effective for brain injuries:
HBOT for the treatment of brain stem injuries has several functions and advantages:
Rapid Oxygen Increase:HBOT quickly increases the body's oxygen levels, improving oxygen deficiency symptoms in brain tissues and facilitating brain function recovery.
Reduction of Brain Edema:HBOT can alleviate brain edema and improve intracranial pressure symptoms.
Activation of the Reticular Activating System:HBOT can activate the central reticular activating system, significantly aiding in the arousal of coma patients.
Establishment of Collateral Circulation: It can help establish collateral circulation in brain tissues, improving blood supply and oxygen delivery to the brain.
Hyperbaric oxygen therapy can be an effective treatment for brain injuries. It provides oxygen directly to the brain, mitigates the respiratory effects on brain tissues, and supports metabolic processes in the body. Generally, younger patients tend to respond better to treatment.
It's important to note that the effectiveness of HBOT soft chamber may vary depending on the type and severity of the brain injury, so treatment decisions should be made in consultation with healthcare professionals as part of a comprehensive care plan.
Brain injuries are often caused by external pressure or impact, resulting in the death of some brain cells and a lack of sufficient oxygen absorption in the brain. The use of a hyperbaric oxygen chamber can quickly increase the body's oxygen levels, improve symptoms of brain tissue cell hypoxia, and aid in brain function recovery. Hyperbaric oxygen therapy can reduce brain swelling, improve intracranial pressure symptoms, activate the central reticular system, significantly promote the awakening of comatose patients, establish collateral circulation in brain tissue, and enhance blood and oxygen supply to the brain. Providing sufficient oxygen to the brain accelerates the repair of brain cells and can reduce long-term sequelae.
Both domestic and international experiments have demonstrated the beneficial reparative effects of hyperbaric oxygen therapy for brain injuries, both in basic animal experiments and clinical trials involving human subjects. In human trials, patients using hyperbaric oxygen chambers experienced faster recovery and showed no long-term complications compared to those who did not use hyperbaric oxygen chambers.
Patients with brain injuries, especially in the early stages, often experience brain swelling. Brain edema can compress arteries, reducing perfusion, causing distant hypoxia, and compressing veins, exacerbating local edema. Brain edema increases the distance between capillaries, preventing cells farther from blood vessels from receiving sufficient oxygen for aerobic metabolism, leading to reduced ATP production, channel inactivation, changes in active centers, and cell death.
Professor Liu Qingle explained, "Under normal circumstances, the effective radius of oxygen diffusion in gray matter capillaries of the human brain is only 30 micrometers. When oxygen is administered at 3.0 ATA pressure, we found that the effective radius of oxygen diffusion in gray matter capillaries of the human brain can reach 100 micrometers." Therefore, hyperbaric oxygen therapy can effectively alleviate hypoxia caused by brain edema, reducing the number of damaged and dead brain cells.
Hyperbaric oxygen therapy can also activate the ascending activation system of the brainstem, benefiting comatose patients. Additionally, hyperbaric oxygen therapy can cause blood vessels to contract, similar to the effect of α-adrenaline, which can shrink arteries at the edematous site, reduce local blood volume, and alleviate edema. Despite the reduced arterial blood flow, the high oxygen content in the blood still increases tissue oxygenation. Therefore, hyperbaric oxygen's unique advantage in treating edema in various locations is irreplaceable.
Under hyperbaric conditions, oxygen therapy can increase the permeability of the blood-brain barrier. Generally, when a patient has an intracranial infection, doctors administer antibiotics. If hyperbaric oxygen therapy is simultaneously performed, higher concentrations of antibiotics can accumulate at the infected central site, achieving better anti-inflammatory and antimicrobial effects. Similarly, when a patient has a brain tumor, chemotherapy drugs are administered, and hyperbaric oxygen therapy can enhance the accumulation of chemotherapy drugs at the tumor site, improving the efficacy of anti-tumor chemotherapy.
Hyperbaric oxygen therapy can reduce the size of infarctions. Professor Liu Qingle stated that brain cells are not regenerable after death, and after brain injury, the central area of the infarction lacks oxygen supply, leading to the death of a large number of brain cells. In this region, many cells are only damaged but not dead, and if brain injury patients receive hyperbaric oxygen therapy early, the aerobic metabolism of cells in the damaged area will rapidly recover, reducing cell death and improving prognosis. Conversely, prolonged hypoxia in brain cells leads to increased cell death and worse prognosis.
Scientific Evidence
The U.S. government website indicates that HBOT has significant therapeutic effects on patients with brain injuries:
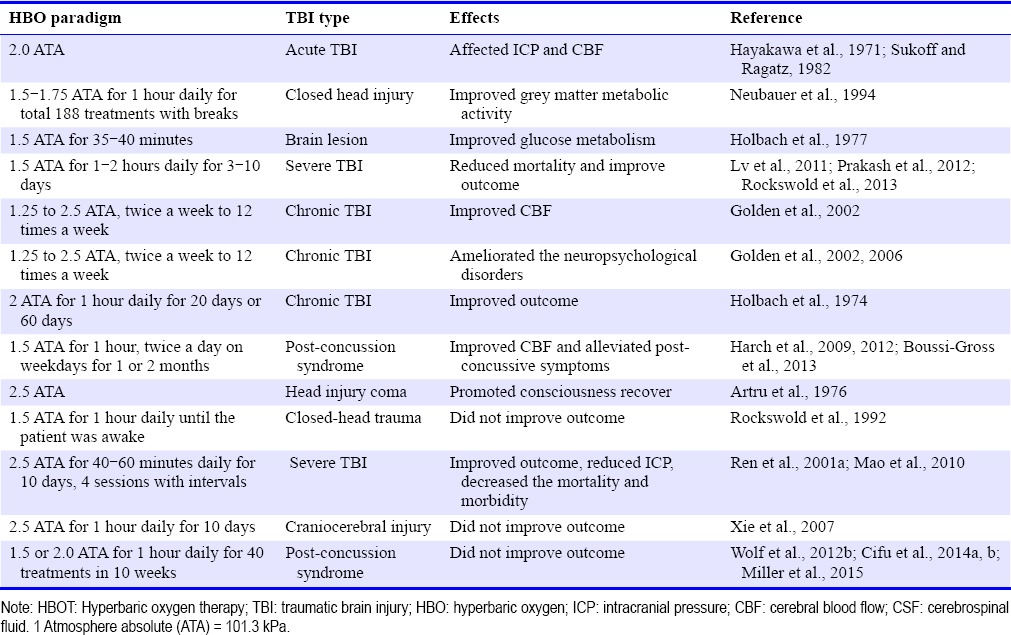
Clinical studies on HBOT treatment of TBI patients.
CASE VIGNETTE
RP is a 55-year-old man who originally entered treatment with a 20-year history of bipolar disorder. His life had been chaotic because of lack of treatment adherence. He was stabilized on a modest dose of lithium and has been in a stable relationship and successfully self-employed for the past 10 years.
When it occurred to me to ask him about concussions, it emerged that there were several significant sports-related concussions during adolescence and at least a half-dozen serious concussions in early adulthood, possibly related to recklessness during manic episodes. His last concussion occurred 30 years before this history was obtained. He was unable to describe any specific post-concussion symptoms, possibly because he had so many concussions starting in adolescence, and could not remember what his functioning was like prior to his concussions. A brain-perfusion SPECT scan showed extensive perfusion defects consistent with TBI, which is a strong predictor of clinical benefit with HBOT. Accordingly, he was offered treatment even in the absence of a clear history of acquired symptoms.
The patient rented a mild-HBOT chamber and did the treatment at home. He completed two blocks of 40 one-hour sessions of mild HBOT (1.3 ATM, 100% O2) over the course of 4 months. A post-treatment SPECT scan was obtained about 56 months after he completed the treatment protocol.
Following is the summary section of the radiologist report for each scan. Note that a normal SPECT scan should show homogeneous perfusion, whereas areas of reduced perfusion or heterogeneous (spotty) perfusion indicate cortical areas of reduced blood flow.
Pre-treatment SPECT scan,
Aug. 29, 2016
“Findings: Decreased tracer perfusion is seen in the right temporal lobe and also there is heterogeneous perfusion in the bilateral parietal and posterior frontal lobes. The cerebellar hemispheres are symmetrically perfused in the correct clinical settings, this may reflect sequelae of traumatic brain injury.”
Post-treatment SPECT scan,
Dec. 27, 2017
“Findings: Brain SPECT images demonstrate homogeneous perfusion of the cerebral hemispheres. There are no asymmetric perfusion defects, with interval resolution of previously seen asymmetrically decreased radiotracer uptake in the right temporal lobe. Similarly, previously seen decreased perfusion in bilateral parietal and posterior frontal lobes has resolved. Impression: Normal brain perfusion SPECT with interval resolution of previously seen areas of decreased perfusion.”
After completing treatment he reported improvement in focus, improved ability to multitask, and generally more stable emotional functioning. He noted that he was using vocabulary that he had not used since he was a teenager, which was readily observable on interview. He found that he was communicating with people in a much more direct way, in contrast to his usual tendency to be tangential with difficulty getting to the point. He stopped using an appointment book for his business, finding that he could keep track of appointments with his clients for several weeks ahead by memory.
Background: Mild traumatic brain injury results in over 15% of patients progressing to Persistent Postconcussion Syndrome, a condition with significant consequences and limited treatment options. Hyperbaric oxygen therapy has been applied to Persistent Postconcussion Syndrome with conflicting results based on its historical understanding/definition as a disease-specific therapy. This is a systematic review of the evidence for hyperbaric oxygen therapy (HBOT) in Persistent Postconcussion Syndrome using a dose-analysis that is based on the scientific definition of hyperbaric oxygen therapy as a dual-component drug composed of increased barometric pressure and hyperoxia.
Methods: In this review, PubMed, CINAHL, and the Cochrane Systematic Review Database were searched from August 8–22, 2021 for all adult clinical studies published in English on hyperbaric oxygen therapy in mild traumatic brain injury Persistent Postconcussion Syndrome (symptoms present at least 3 months). Randomized trials and studies with symptomatic and/or cognitive outcomes were selected for final analysis. Randomized trials included those with no-treatment control groups or control groups defined by either the historical or scientific definition. Studies were analyzed according to the dose of oxygen and barometric pressure and classified as Levels 1–5 based on significant immediate post-treatment symptoms or cognitive outcomes compared to control groups. Levels of evidence classifications were made according to the Centre for Evidence-Based Medicine and a practice recommendation according to the American Society of Plastic Surgeons. Methodologic quality and bias were assessed according to the PEDro Scale.
Results: Eleven studies were included: six randomized trials, one case-controlled study, one case series, and three case reports. Whether analyzed by oxygen, pressure, or composite oxygen and pressure dose of hyperbaric therapy statistically significant symptomatic and cognitive improvements or cognitive improvements alone were achieved for patients treated with 40 HBOTS at 1.5 atmospheres absolute (ATA) (four randomized trials). Symptoms were also improved with 30 treatments at 1.3 ATA air (one study), positive and negative results were obtained at 1.2 ATA air (one positive and one negative study), and negative results in one study at 2.4 ATA oxygen. All studies involved <75 subjects/study. Minimal bias was present in four randomized trials and greater bias in 2.
Conclusion: In multiple randomized and randomized controlled studies HBOT at 1.5 ATA hyperbaric chamber demonstrated statistically significant symptomatic and cognitive or cognitive improvements alone in patients with mild traumatic brain injury Persistent Postconcussion Syndrome. Positive and negative results occurred at lower and higher doses of oxygen and pressure. Increased pressure within a narrow range appears to be the more important effect than increased oxygen which is effective over a broad range. Improvements were greater when patients had comorbid Post Traumatic Stress Disorder. Despite small sample sizes, the 1.5 ATA HBOT studies meet the Centre for Evidence-Based Medicine Level 1 criteria and an American Society of Plastic Surgeons Class A Recommendation for HBOT treatment of mild traumatic brain injury persistent postconcussion syndrome.

Discount Price, ship by DHL, door to door service, 5-7days delivery time, local technical support

We supply soft and hard chambers from 1.3-2.0ATA to reach different customers' needs

Create custom uniquea hyperbaric chambers to reach your target market

We have more than 50 distributors around world, looking forward to having you on board.